Cronkite News has moved to a new home at cronkitenews.azpbs.org. Use this site to search archives from 2011 to May 2015. You can search the new site for current stories.
Rising access to substance abuse treatment faces shortage of counselors
WASHINGTON – Changes to health care law in the past year gave millions of Americans access to mental health and substance abuse treatment, but did nothing to address a shortage of professionals who can provide that care.
Experts say the shortage of providers has reached “crisis” levels, and there is little indication that their numbers will increase to keep pace with the demand.
“We have a shortage all across the country. I can’t point to a state where it’s not a problem,” said Becky Vaughn, vice president of addictions at the National Council for Behavioral Health.
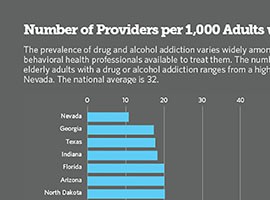
The problem could be particularly acute in Arizona, which had just 20 substance abuse professionals per 1,000 adults with addictions, the sixth-lowest rate in the nation, according to a new analysis. The national average is 32 per 1,000.
Neal Cash, CEO of the Community Partnership of Southern Arizona, said the workforce shortage is getting “more severe and more critical.”
“As more people have health care that includes mental health and substance abuse benefits, that’s compounding a situation that was already there,” Cash said.
In 2013, only 18 percent of adults with substance abuse disorders got treatment, according to a study by the Pew Research Center, in part because of a lack of insurance coverage.
But in 2014, as many as 60 million Americans got access to new or expanded behavioral health benefits, which includes substance abuse treatment, due to two federal laws, the Substance Abuse and Mental Health Services Administration said.
The Affordable Care Act, better known as Obamacare, named substance abuse disorders as one of 10 essential health benefits that must be cover
ed by Medicaid and by any insurance plan sold through a health care marketplace.
And the Mental Health Parity and Addiction Equity Act mandated that, as of 2014, insurance companies could no longer treat behavioral health care differently than primary care by charging higher copays or limiting the number of treatments patients can receive.
The new laws mean that mental health and substance abuse can no longer be treated “as a stepchild,” said Jeff Zornitsky, director of strategic initiatives at Advocates for Human Potential, a research firm specializing in health and behavioral health.
“They have to be treated the same way as people with, say, diabetes,” he said.
Advocates welcomed those changes, but predict they will overwhelm an already strained workforce.
According to data compiled by Zornitsky, the number of substance abuse specialists per 1,000 adults with addictions ranges from a low of 11 in Nevada to a high of 70 in Vermont. He said Arizona falls in the bottom quartile of states.
“These folks in Arizona are probably going to have a tougher time meeting need than places that were at the top of the heap,” Zornitsky said. “Access to care suffers.”
And Vaughn said access is critical for people with behavioral health problems like substance abuse disorders, who need “treatment on demand.”
“People say, ‘What’s the waiting list for that facility?’ There’s no waiting list,” Vaughn said. “When people come in and they are addicted … and they’re seeking help, if you tell them to come again in six weeks, more than likely you’ll never see them again.”
But the industry has had a hard time recruiting and retaining a workforce in part because workers make less money than their counterparts in other health care areas, Vaughn said.
“We lose a lot of people,” she said. “The burnout rate, as you can imagine, is tremendous – low pay, long hours, working with difficult people. It’s hard to inspire people to want to work with people who are addicted to alcohol or drugs.”
By 2020, Arizona will have 4,900 behavioral health jobs to fill, Zornitsky said. Nationally, there will be about 300,000 jobs that need filling.
Cash said licensed substance abuse workers will likely be overwhelmed as demand for service increases, affecting the quality of care patients receive.
“If you’re seeking help and you need help, you don’t want to be shortchanged and you want to be able to get the kind of care that you need,” Cash said.
“I would say that for the most part that occurs, but as the system gets more strained, the demand exceeds the capacity to effectively treat people, and that could certainly become a problem,” he said.